A scaly hand rash can be fungus (tinea manuum) or eczema. Getting it right matters because treatments differ.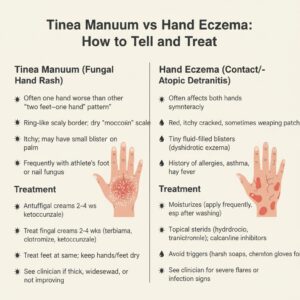
Tinea Manuum (Fungal Hand Infection)
- Clues it’s fungus:
- Usually one hand worse than the other (“two feet–one hand” pattern if athlete’s foot is present).
- Ring-like, expanding scaly border on the palm or back of hand; can be dry and “moccasin-like” on the palm with fine scale.
- Itches; may have small blisters.
- Often coexists with tinea pedis (athlete’s foot) or nail fungus.
- Tests:
- A clinician can scrape scale for a KOH exam or culture to confirm.
- Treatment:
- Topical antifungals 2–4 weeks (terbinafine, butenafine, clotrimazole, ketoconazole).
- For thick, chronic, or widespread cases, oral antifungals (terbinafine/itraconazole) may be needed.
- Treat feet at the same time to prevent reinfection. Clean/disinfect shared items; keep hands/feet dry.
Hand Eczema (Dermatitis)
- Clues it’s eczema:
- Both hands (often), history of atopic dermatitis or sensitive skin.
- Itchy, dry, cracked areas; may have tiny blisters on sides of fingers (dyshidrotic eczema).
- Flares with soaps, wet work, cold weather, or specific products (possible contact allergy).
- Treatment:
- Gentle care: fragrance-free cleanser, moisturize after every wash with thick creams/ointments.
- Short courses of topical steroids for flares; non-steroid anti-inflammatories for maintenance.
- Patch testing if allergic contact dermatitis is suspected.
Quick tip to differentiate
- Unilateral scaly annular patch with active border + athlete’s foot = think tinea.
- Symmetric dry, fissured hands worse with washing/chemicals = think eczema.
When to see a clinician
- If home antifungal or eczema care fails after 2–4 weeks.
- Painful cracks, signs of infection (pus, yellow crust, fever).
- To test and choose targeted therapy.
Prevention
- Keep hands dry between fingers; use cotton glove liners under nitrile for wet work.
- Don’t share towels; clean gym gear; wear sandals in locker rooms.
- Moisturize routinely; avoid harsh soaps.
